- Received November 30, -0001
- Accepted November 30, -0001
- Publication August 18, 2020
- Visibility 10 Views
- Downloads 1 Downloads
- DOI 10.18231/j.ijpi.2020.012
-
CrossMark
- Citation
Revisit to endo-perio lesion a review
- Author Details:
-
Roopali Sharma *
-
Akshita Gupta
-
K K. Gupta
-
Sarah Jameel
-
Rashmika Kapoor
Introduction
Inter relationship between pulpal and periodontal tissues has been a point of interest since years now. Simring and Goldberg were the first to reflect on the relationship between periodontal and pulpal disease in 1964. This article will lead you to the information regarding association of pulpal and periodontal tissues in the same dental structure.
Microbiology
The flora dominating the concerned lesion varies in endodontic and periodontal diseases. Yet some are seen shairing the enviornment. [1] The flora in the tooth with periodontal pockets were mostly rods and motile organisms and those in the root canals were largely rods and cocci. [2] Bacteria such as Actinobacillus actinomycetemcomitans, bacteroides frosythus, Ekinella corrodens, Fusobacterium nucleatum, Porphyromonas gingivalis, Prevotella intermedia and Treponema denticola are discovered in teeth with endodontic disease chronic apical periodontitis and chronic adult periodontitis.
Fungal species like Candida albicans were also present both in endodontic infections as well as in subgingivally patients with adult periodontitis. Cytomegalo virus, Epstein-Barr virus, herpes virus may be involved in causing of periodontal and endodontic disease ranging from an increase in periodontal pathogens in periodontal pockets to involvement in pulpal and periapical diseases.
Pathway of endo-perio relationship
Dental pulp and periodongtal structure share embryonic, anatomical and functional connection. They both are ectomesenchymal in origin.
Anatomically: via the apical foramina, dentinal tubules, and lateral or accessory canals. Pulpal inflammation can cause inflammatory changes in the periodontal ligament even before the pulp becomes totally necrotic.
Following can serve as potential predisposing factors:
Mal-alignment of a tooth
Presence of a multirooted tooth in a position usually occupied by a single rooted tooth, or additional roots, separate or fused in multirooted teeth.
Presence of additional canals and changes in root structure in single and multirooted teeth.
Cervical enamel projections into the furcation of multirooted teeth.
Large lateral (accessory) canals in coronal and middle sections ofroots.
Trauma
Trauma is a major etiologic factor in the formation of
an endodontic – periodontic lesion. i. Combined with gingival inflammation, trauma can lead to deep periodontal pockets or, in multirooted teeth, furcation exposure.
There is a marked difference in canals of tooth treated with endodontic therapy than i9n untreated teeth especially in terms of flora. [3]
Under a study Blomlof et al concluded that endodontic infection promotes periodontal pocket formation . Thus, root canal disinfection is crucial when attempting to achieve regeneration of the periradicular tissues. [4]
Classification: [5], [6]
The periodontal-endodontic lesions have various classifactions.
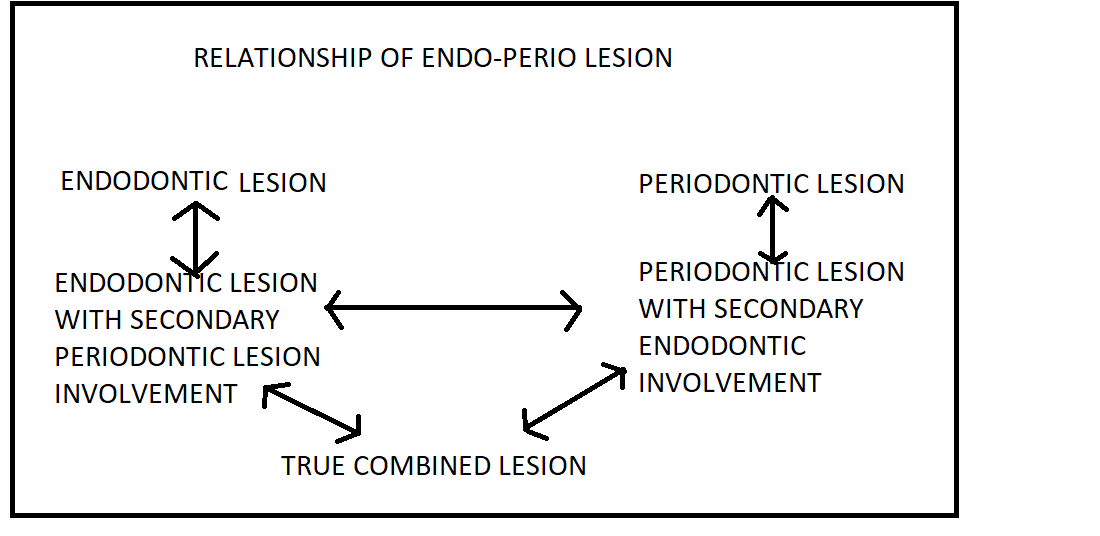
Classification by Simon et al:-
(i) Primary endodontic lesions,
(ii) Primary endodontic lesions with secondary periodontal involvement,
(iii) Primary periodontal lesions,
(iv) Primary periodontal lesions with secondary endodontic involvement,
(v) True combined lesions.
Classification by Torabinejad and Trope in 1996 based on the origin of the periodontal pocket:
(i) Endodontic origin,
(ii) Periodontal origin,
(iii) Combined endo-perio lesion,
(iv) Separate endodontic and periodontal lesions,
(v) Lesions with communication,
(vi) Lesions with no communication.
Classification recommended by the world workshop for classification of periodontal diseases (1999), Periodontitis Associated with Endodontic Disease:
(i) endodontic-periodontal lesion,
(ii) periodontal-endodontic lesion,
(iii) combined lesion.
In 2014,[7] Al-Fouzan[4] suggested a new endodontic-periodontal interrelationship classification, based on the primary disease and its secondary effect.
(1) Retrograde periodontal disease
(a) Primary endodontic lesion with drainage through the periodontal ligament
(b) Primary endodontic lesion with secondary periodontal involvement
(2) Primary periodontal lesion
(3) Primary periodontal lesion with secondary endodontic involvement
(4) Combined endodontic-periodontal lesion
(5) Iatrogenic periodontal lesion
Diagnosis: [8]
The endo-perio lesions present challenges to clinicians as far as diagnosis and prognosis of the involved teeth are concerned. Correct diagnosis is half the case solved. Proper history taking is a crucial step towards effective treatment of the disease. Following are the methods to be considered:-
Visual examination
Visual examination includes the examination for the presence of inflammation and ulcerations or sinus tract in alveolar mucosa and attached gingiva. The necrotic pulp is associated with sinus tract. [9]
Pain
Various aspects of pain should be considered when differentiating between pulpal and periodontal disease (type, intensity, frequency, duration, and activators of pain).
Swelling
Swelling by pulpal infections :often in the
mucobuccal folds or spreads to the facial planes.
Swelling by periodontal infection: often in the attached gingival and rarely spreads beyond the mucogingival junction and usually does not cause facial swelling.
Suppuration or abscess formation:
Of periodontal disorders: may be linked with an acute periodontal abscess, a chronic periodontal disease, or an acute exacerbation of a chronic disorder.
Of pulpal disorder: may be with either an acute or chronic condition such as an acute alveolar abscess or a chronic alveolar abscess draining through a fistula.
Probing
Use of gutta-percha point or a fine wire inserted into the orifice of the fistula reveals the source.
Vitality tests:[10]
The ability of vitality tests to detect non-sensitive reaction represented a necrotic pulp was reported as 89% with the cold test and 88% with the elec-trical test.
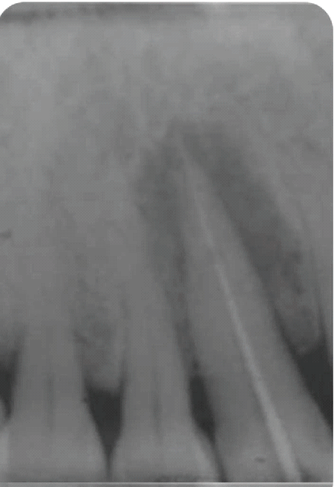
Radiograph
Different level of bone losses may be seen in endodontic lesions.[11][12] The radiographic appearence of combined endo-perio disease maybe similar to vertical root fracture.
Diabetes and endo-perio lesion
Diabetes mellitus affects the condition of the masticatory organ, and thus periodontium. [13]
In diabetic patients, aging changes of pulp due to limited collateral blood flow are faster than nondiabetics. Since diabetes damages the blood circulation or ischemia, sometimes necrosis of pulp may occur. [14]
Treatment
The endo-perio lesion has represents a lesion whose characterising damage is coexisting with endodontic infection and periodontic damage.[15] [16]Before the commencement of any kind of advanced restorative work to treat a perio-endo lesion, extraction of the tooth should be considered as an alternative. Radiographs can help revealing guidelines to the treatment.
Endodontic Lesion
When the aetiology is purely endodontic, calcium hydroxide can be used as an intracanal medicament. Because of its bactericidal, anti-inflammatory and proteolytic properties, it inhibits resorption and favors repair It is especially effective in endodontic lesions with extensive periapical pathology and pseudo pockets, because of its temporary obturating action which would prevent periodontal contamination of the instrumented canals via patent channels of communication. [17]
Primary endodontic disease with secondary[20]
periodontal involvement should first be treated with endodontic therapy. Treatment results should be
evaluated in 2-3 months and only then should periodontal treatment be considered.
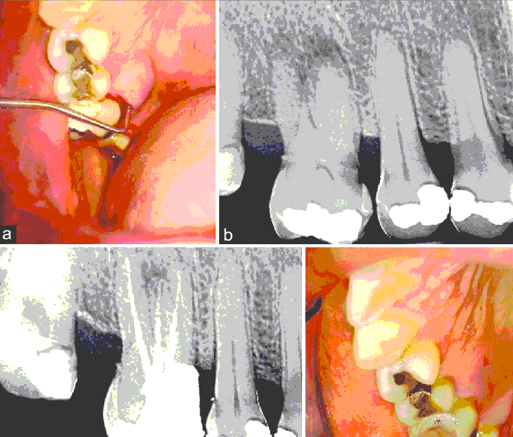
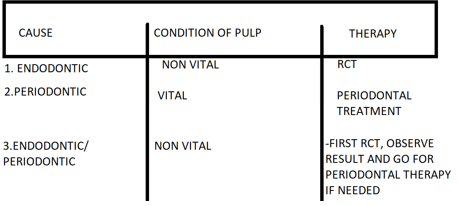
Picture above representing primary endodontic case with secondary involvement of periodontal problem.

Endo-perio case radiograph.
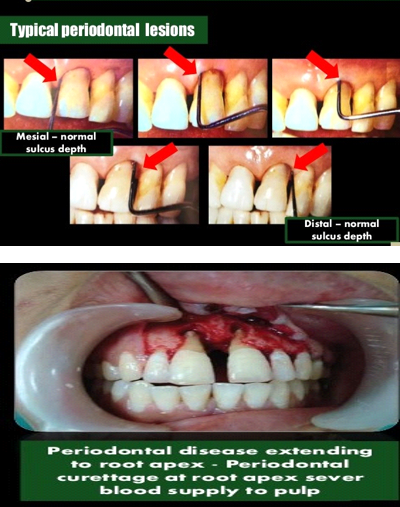
Periodontic Lesion
Primary periodontal lesions are treated by hygiene phase therapy initially. Periodontal surgery is performed after the completion of hygiene phase therapy if needed.
Early stage periodontal lesions with secondary endodontic involvement, with limited reversible pulpal hypersensitivity, may be treated by periodontal therapy only. [18]
The most important factor in the treatment is a correct diagnosis. Specific things to look for in the history include past disease, trauma and pain. This will reveal better strategy for the next step.[19]
True Combinedn Lesion
This lesion forms when endodontic disease progress coronally and joins with infected periodontal pocket progressing apically. [20] [21]Alternative for endo-perio lesion management is anatomical redesigning like Root amputation, tooth resection and Bicuspidization.[22] In molar teeth root resection can be effective if all roots are not severly damage

Picture above representing a case which is periodontally Compromised and Endodontically Involved Three- Rooted Mandibular First Molar With Cervical Enamel Projection.
Outline of treatment strategy to be followed when there is doubt over the origin of lesion: [23]
Prognosis: [24]
The prognosis of periodontal lesions is poorer than endodontic lesion and is dependent on the apical extension of the lesion. [25] The prognosis of an affected tooth can also be improved by increasingly bone support which can be achieved by bone grafting and guided tissue regeneration. This is due to the most critical determinant of prognosis being a loss of periodontal support.
The low failure rate are observed when antimicrobial strategy is implemented during endodontic treatment of teeth with apical periodontitis. [26]
Platelet-Rich Plasma
[27] To overcome healing limitations in endo-perio lesions use of purified growth factor to stimulate patients own cells towards a regenerative response has been tested. [28]The positive impact of PRF on bone healing could be attributed to the angiogenic, proliferative and differentiating effects on osteoblasts of tissue growth factor β and platelet derived growth factor (TGF-β and PDGF) that are present in PRF in high concentrations.This has resulted in promisig results, though some potetntial risk factors are associated with it.[29] The prognosis of the lesion depends on the severity of the disease, efficacy of the therapy and response of the patient.
Conclusion
Endo- perio lesion can be challenging case espically when considered in the terms of the origin of lesion. Proper history taking and careful diagnosis can help in providing better strategy to the treatment. Further advancement in dentistry such as use of PRF has expanded the boundaries of treatment.
Source of Funding
None.
Conflict of Interest
None.
References
- H Kurihara, Y Kobayashi, I A Francisco, O Isoshima, A Nagai, YMurayama. A microbiological and immunological study of endodontic-periodontic lesions. J Endod 1995. [Google Scholar]
- S W Peeran, M Thiruneervannan, K A Abdalla, M H Mugrabi. Endo-perio lesions. Int J Sci Technol Res 2013. [Google Scholar]
- Göran Sundqvist, David Figdor, Sten Persson, Ulf Sjögren. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endodontol 1998. [Google Scholar]
- R Kumar, S Patil, U Hoshing, A Medha, R Mahaparale. Non-surgical endodontic management of the combined Endo-perio lesion. Int J Dent Clin 2011. [Google Scholar]
- James H.S. Simon, Dudley H. Glick, Alfred L. Frank. The Relationship of Endodontic–Periodontic Lesions. J Endod 2013. [Google Scholar]
- Khalid S. Al-Fouzan. A New Classification of Endodontic-Periodontal Lesions. Int J Dent 2014. [Google Scholar]
- H Alquthami, A M Almalik, F F Alzahrani, L Badawi. Successful management of teeth with different types of endodontic-periodontal lesions. . Case Rep Dent 2018. [Google Scholar]
- VSunitha Raja, Pamela Emmadi, Ambalavanan Namasivayam, Ramakrishnan Thyegarajan, Vijayalakshmi Rajaraman. The periodontal - endodontic continuum: A review. J Conserv Dent 2008. [Google Scholar]
- G Dahlen. Microbiology and treatment of dental abscesses and periodontal-endodontic lesions. Periodontol 2000. [Google Scholar]
- H. Aksel, A. Serper. A case series associated with different kinds of endo-perio lesions. J Clin Exp Dent 2014. [Google Scholar]
- James H. S. Simon, Dudley H. Glick, Alfred L. Frank. The Relationship of Endodontic-Periodontic Lesions. J Periodontol 1972. [Google Scholar]
- I Rotstein, J H Simon. The endo-perio lesion: a critical appraisal of the disease condition. Endod Top 2006. [Google Scholar]
- E Preferansow, M Gołebiewska, E Kulikowska-Bielaczyc, M Górska. The assessment of periodontium in patients with uncontrolled diabetes. Adv Med Sci 2006. [Google Scholar]
- S Dhoum, K Laslami, F Rouggani, El Ouazzani, A Jabri, M. Endo-perio lesion and uncontrolled diabetes. . Case Rep Dent 2018. [Google Scholar]
- A Bonaccorso, T R Tripi. Endo-perio lesion: Diagnosis, prognosis and decision-making. . END0 (Lond Engl) 2014. [Google Scholar]
- Vishal Anand, Vivek Govila, Minkle Gulati. Correlation of gingival tissue biotypes with gender and tooth morphology: A randomized clinical study. Indian J Dent 2012. [Google Scholar]
- Sharnappa Kambale. A Sequential Approach in Treatment of Endo-Perio Lesion A Case Report. J Clin Diagn Res 2014. [Google Scholar]
- Ashutosh Nirola, Sunanda Grover, Ajay Sharma, Damanjeet Kaur. Pulpal perio relations: Interdisciplinary diagnostic approach - I. J Indian Soc Periodontol 2011. [Google Scholar]
- P Singh. Endo-perio dilemma: a brief review. Dent Res J 2011. [Google Scholar]
- A Suchetha, Salman Khawar, N Sapna, S M Apoorva, B M Darshan, Divya Bhat. Endo-perio lesion: A case report. Int J Appl Dent Sci 2016. [Google Scholar]
- A Arora, V Mehta, V Goyal, V Sharma, M Gupta. Fundamentals in Treatment of Endo-Perio Lesions-A Review. Int J Dent Clin 2012. [Google Scholar]
- I Rotstein, J H Simon. The endo-perio lesion: a critical appraisal of the disease condition. Endod Top 2006. [Google Scholar]
- Sharnappa Kambale. A Sequential Approach in Treatment of Endo-Perio Lesion A Case Report. J Clin Diagn Res: JCDR 2014. [Google Scholar]
- Ashutosh Nirola, Sunanda Grover, Ajay Sharma, Damanjeet Kaur. Pulpal perio relations: Interdisciplinary diagnostic approach - I. J Indian Soc Periodontol 2011. [Google Scholar]
- Sharnappa Kambale. A Sequential Approach in Treatment of Endo-Perio Lesion A Case Report. J Clin Diagn Res: JCDR 2014. [Google Scholar]
- José F. Siqueira, Isabela N. Rôças, Fernanda N.S.J. Riche, José C. Provenzano. Clinical outcome of the endodontic treatment of teeth with apical periodontitis using an antimicrobial protocol. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endodontol 2008. [Google Scholar]
- NB Nagaveni, KNandini Kumari, P Poornima, VVSubba Reddy. Management of an endo-perio lesion in an immature tooth using autologous platelet-rich fibrin: A case report. J Indian Soc Pedod Prev Dent 2015. [Google Scholar]
- L Goyal. Clinical effectiveness of combining platelet rich fibrin with alloplastic bone substitute for the management of combined endodontic periodontal lesion. . Restor Dent Endod 2014. [Google Scholar]
- A Suchetha, Dr, A Suchetha, Dr Salman Khawar, Dr Sapna, N, Dr Apoorva, S M, Dr Darshan, Dr. Divya Bm, Bhat. . . [Google Scholar]
- Introduction
- Microbiology
- Pathway of endo-perio relationship
- Trauma
- Classification: [5], [6]
- Diagnosis: [8]
- Radiograph
- Treatment
- Endodontic Lesion
- Primary endodontic disease with secondary[20]
- Endo-perio case radiograph.
- Periodontic Lesion
- True Combinedn Lesion
- Prognosis: [24]
- Platelet-Rich Plasma
- Conclusion
- Source of Funding
- Conflict of Interest
