- Visibility 137 Views
- Downloads 34 Downloads
- DOI 10.18231/j.ijpi.2021.031
-
CrossMark
- Citation
Peripheral ossifying fibroma: A case report
- Author Details:
-
Sandip Ghosh *
-
Balaji R
-
Ashit Kumar Pal
-
Somen Bagchi
-
Sandip Ghose
Introduction
Various localized reactive lesions are seen on the gingiva which include Pyogenic granuloma, Peripheral giant cell granuloma, Focal fibrous hyperplasia and Peripheral Ossifying Fibroma (POF).[1] Though pyogenic granuloma is one of the most commonly occurring gingival overgrowth in gingiva but peripheral ossifying fibroma also found in anterior tooth region. POF, also known as peripheral cementifying fibroma, peripheral fibroma with cementogenesis, peripheral fibroma with osteogenesis, peripheral fibroma with calcification, calcified or ossified fibrous epulis, and calcified fibroblastic granuloma infrequently occurring focal, reactive, non-neoplastic tumor-like growth of the soft tissue that primarily arises from the interdental papilla may arise as a result of such irritants as trauma, microorganisms, plaque, calculus, restorations, and dental appliances.[2], [3], [4] Craniofacial bones are primarily the site for occurring Ossifying fibroma which is generally two types: Central and peripheral. Ossifying fibroma arises from the endosteum or the PDL adjacent to the root apex and expands from the medullary cavity of the bone are categorized as central type and those shows a contiguous relationship with the PDL, occurring solely on the soft tissues overlying the alveolar process are categorized as peripheral type.[5], [6] The present article highlights a case report related to peripheral ossifying fibroma in a 32-year male patient, its diagnosis, satisfactory clinical management along with future treatment planning.
Case Report
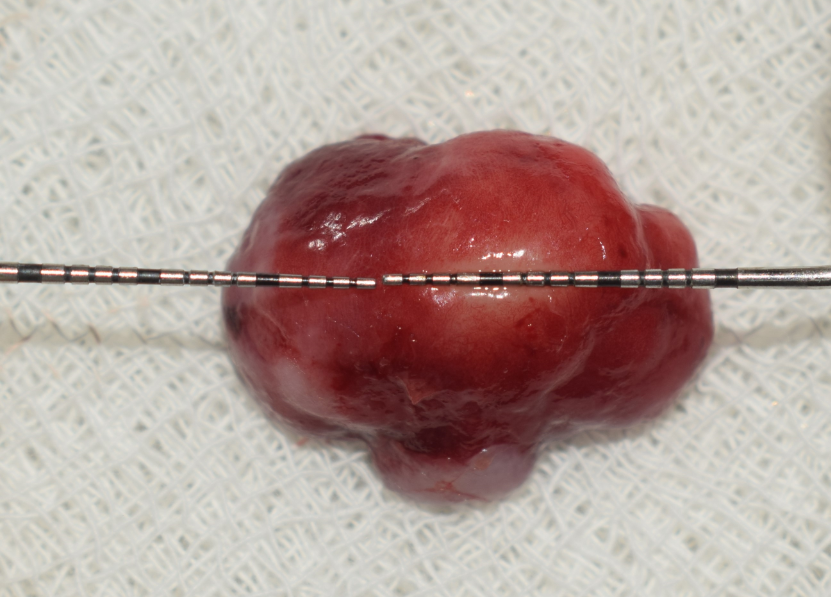
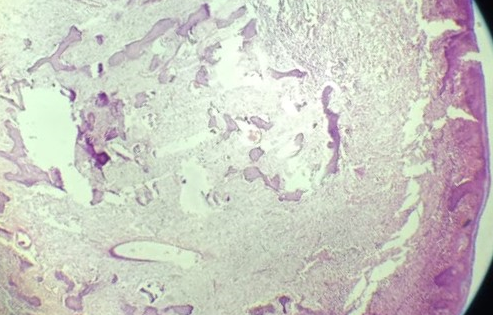
A 32-year-old female patient was reported to the department of Periodontology with the complaint of swelling & discomfort while eating and speaking due to a growth in the upper front teeth region. History dates back to 8 months when patient first noticed a single nontender small nodule which was increases in size after that till date of presentation. No relevant history of bleeding or pain, no significant medical history and no history of any medication was recorded at that time. Intraoral examination revealed firm, erythematous, non-hemorrhagic, non-tender, blanched on pressure and pedunculated solitary oval growth present on the interdental and marginal gingiva of the upper right central & lateral incisor i.e. 11 & 12 measuring about 15mm x 15mm. [[Figure 1]] POF, peripheral giant cell granuloma, gingival fibroma, pyogenic granuloma, peripheral odontogenic fibroma were noted as differential diagnosis. Hematological investigation was done including complete blood picture and blood glucose and all the reports was normal. radiological investigation through IOPA radiograph was done and it revealed that there was interdental bone loss around the RCT treated 11[[Figure 4]]. Patient education and motivation, Oral hygiene instructions, thorough scaling and root planing, reevaluation and surgical excision of the lesion under local anesthesia are planned after clinical, hematological and radiological examination. On the appointment day of supragingival ultrasonic scaling careful selective grinding was done to make that tooth trauma free and to eliminate the local irritants. After 15 days of SRP reevaluation done and planned for surgical excision. Complete surgical removal of the growth along with deep curettage was done under local anesthesia [[Figure 2]] and non eoginol base COE –PAK periodontal dressing was placed. Patient was given post-operative instructions and was prescribed with analgesic (Tablet Ibuprofen400mg tid) and mouth rinse (0.2% chlorhexidine gluconate twice-a-day for 1 week). She was recalled, after 1 week for follow-up. The excised tissue [[Figure 3]] was placed in 10% neutral buffered formalin and sent for the histopathological examination. On histopathological examination, low power magnification (4x) showed a keratinized stratified squamous epithelium (gingiva), overlying a fibrous interlacing collagen bundles and numerous ossifications. This picture is consistent with the clinical diagnosis of POF. [[Figure 5]] At 1 week post-operative visit, patient presented for periodontal dressing removal and follow-up examination. There was a satisfactory healing [[Figure 6]]. Patient is on regular follow-up. There was no recurrence at 3 months follow up. [[Figure 7]]





Discussion
The term peripheral ossifying fibroma was originally coined by Gardner in 1982 and described POF as a lesion that is reactive in nature and is not the extra osseous counterpart of a COF of the maxilla and mandible.[3] Since the late 1940s Intraoral ossifying fibromas have been described in the literature and several terms are used like - epulis, peripheral fibroma with calcification, POF, calcifying fibroblastic granuloma, peripheral cementifying fibroma, peripheral fibroma with cementogenesis and peripheral cemento-ossifying fibroma to describe similar type of lesions. The mere number of names used for fibroblastic gingival lesions in literature indicates there was much controversy regarding the classification of these types of lesions.[6], [7] Jacoway JR in 1966 in his report of 376 cases suggested POF represents a separate clinical entity rather than a transitional form of pyogenic granuloma, PGCG, or irritation fibroma.[8] According to Eversole and Rovin the similar sex and site predilection of pyogenic granuloma, PGCG and POF, as well as similar clinical and histological features, these lesions may simply be varied histological responses to irritation.[9] Regardless of the presence or absence of calcification cellular connective tissue is so characteristic in POF that a histological diagnosis can be made with confidence with that as stated by Gardner in 1982.[3]
According to Buchner and Hansen’s hypothesis POF may be misdiagnosis as a pyogenic granuloma as it in its early situation presents as ulcerated nodules with mild calcification.[10]
Areas like skull, femur, and tibia where there is no cementum clinical presentation and histopathology of cemento-ossifying fibroma are the same (all are ossifying fibroma) so the term cemento ossifying scientifically inaccurate. It is clear that the term cemento-ossifying fibroma should not be used merely just because of teeth for the overgrowth in jaw.[11], [12]
Due to presence of oxytalin fibers within the mineralized matrix of most of the lesions, proximity of gingiva to the PDL and exclusive occurrence in gingiva, it is suggested that POF arises from PDL cells but the actual etiopathogenesis of POF is not well discussed. Chronic gingival injury, gingival irritation, sub gingival calculus, or a foreign body in the gingival sulcus may responsible for excessive proliferation of mature fibrous connective tissue in POF. Metaplastic features can also be seen due to presence of chronic irritation to the periosteum and periodontal membrane.
Young females (first and second decades of life, increasing occurrence in the second decade, and declining incidence after the third decade) are suffered more than male from POF as hormonal influence may be an important factor for that occurrence along with other factors. The female and male ratio varies from 1.22:1 and 1.7:1 to 4.3:1.[13], [14]
There may be no significant changes on radiograph in most of the cases but according to degree of mineralization there may be some radiodensity in some cases. CBCT and MRI can be done as an additional investigation for larger lesions.[15], [16]
In this case there is some amount of bone loss in between 11 and 21 which is rare in that type of lesion and may be due to trauma on that tooth 10 years ago when patient got RCT treatment due to Ellis class III fracture .
POF, peripheral giant cell granuloma, gingival fibroma, pyogenic granuloma, peripheral odontogenic fibroma are noted as differential diagnosis. Surgical excision of growth was done under local anesthesia after all clinical hematological and radiological investigation. Deep subgingival curettage is done also along with excision to assure complete removal of the growth. POF was confirmed as a definitive diagnosis through histopathological evaluation. Histologically, the key feature of this lesion is exceedingly cellular mass of connective tissue comprising large number of plump, proliferating fibroblasts intermingled throughout with delicate fibrillar stroma.
According to Buchner and Hansen, 1987 mineralized contents that are found in POF are basically three types:
Bone that may be woven, lamellar or trabecular, sometimes surrounded by osteoid.
Cementum like material that appears as spherical bodies resembling cementum or large acellular round to oval eosinophilic bodies, which seemed to have coalesced to form islands in various sizes and shapes.
Dystrophic calcification, which can range from small clusters of minute basophilic granules or tiny globules to large, solid irregular masses. [10]
Complete surgical excision along with deep periodontal curettage is the treatment of choice suggested by authors and that was performed in our case also. As there was gingival recession and extrusion of tooth to achieve complete treatment for the patient root coverage surgery along with necessary orthodontic correction was planned as future treatment.
Even after surgical removal POF can be occurred again due to persistence of the local irritants, repeated injury, unable to remove completely in during surgery in 8%–20% cases.[17]
Conclusion
Here we present a case report of peripheral ossifying fibroma (POF) clinically which shows similar sign and symptoms like other gingival overgrowth like peripheral fibroma, peripheral giant cell granuloma, and pyogenic granuloma. The only way to confirm the diagnosis of the lesion, histopathological evaluation was done to detect as a POF after surgical excision. POF is a nontender slowly progressive reactive lesion and complete surgical excision along with deep curettage is the treatment of choice to minimize the chances of recurrence. Post surgical follow up for a long term basis is also required for early detection if there are any signs of recurrence.
Conflict of Interest
The authors declare that there are no conflicts of interest in this paper.
Source of Funding
None.
References
- W Zhang, Y Chen, Z An, N Geng, D Bao. Reactive gingival lesions: A retrospective study of 2,439 cases. Quintessence Int 2007. [Google Scholar]
- R E Marx, D Stern. Oral and maxillofacial pathology: a rationale for diagnosis and treatment. 2003. [Google Scholar]
- D G Gardner. The peripheral odontogenic fibroma: An attempt at clarification. Oral Surg Oral Med. Oral Pathol 1982. [Google Scholar] [Crossref]
- B W Neville, D D Damm, C M Allen, J E Bouquot. Oral and Maxillofacial Pathology. 1995. [Google Scholar]
- V P Killi, T Penmatsa, R Narendra. Peripheral ossifying fibroma: A case report. Int J Case Rep Imaging 2012. [Google Scholar]
- L Feller, A Buskin, E J Raubenheimer. Cemento-ossifying fibroma: case report and review of the literature. J Int Acad Periodontol 2004. [Google Scholar]
- R B Zain, Y J Fei. Fibrous lesions of the gingiva: A histopathologic analysis of 204 cases. Oral Surg Oral Med Oral Pathol 1990. [Google Scholar] [Crossref]
- S N Bhaskar, J R Jacoway. Peripheral fibroma and peripheral fibroma with calcification: Report of 376 cases. J Am Dent Assoc 1966. [Google Scholar] [Crossref]
- L R Eversole, S Rovin. Reactive lesions of the gingiva. J Oral Pathol 1972. [Google Scholar]
- A Buchner, L S Hansen. The histomorphologic spectrum of peripheral ossifying fibroma. Oral Surg Oral Med Oral Pathol 1987. [Google Scholar] [Crossref]
- R E Marx, D Stern. Oral and Maxillofacial Pathology: A Rationale for Diagnosis and Treatment. 2012. [Google Scholar]
- D C Shetty, A B Urs, P Ahuja, A Sahu, A Manchanda, Y Sirohi. Mineralized components and their interpretation in the histogenesis of peripheral ossifying fibroma. Indian J Dent Res 2011. [Google Scholar]
- R John, N T Prabhu, A K Munshi. Peripheral ossifying fibroma report of a case. J Indian Soc Pedod Prev Dent 1996. [Google Scholar]
- J N Kenney, G E Kaugars, L M Abbey. Comparison between the peripheral ossifying fibroma and peripheral odontogenic fibroma. J Oral Maxillofac Surg 1989. [Google Scholar]
- A Chatterjee, N Ajmera, A Singh. Peripheral cemento‑ossifying fibroma of maxilla. J Indian Soc Periodontol 2010. [Google Scholar] [Crossref]
- S Chaudhari, H R Umarji. Peripheral ossifying fibroma in the oral cavity: MRI findings. Case Rep Dent 2011. [Google Scholar] [Crossref]
- K Sah, A D Kale, S Hallikerimath, S Chandra. Peripheral cemento‑ossifying fibroma: Report of a recurrence case. Contemp Clin Dent 2012. [Google Scholar]
How to Cite This Article
Vancouver
Ghosh S, R B, Pal AK, Bagchi S, Ghose S. Peripheral ossifying fibroma: A case report [Internet]. IP Int J Periodontol Implantol. 2025 [cited 2025 Sep 08];6(3):179-183. Available from: https://doi.org/10.18231/j.ijpi.2021.031
APA
Ghosh, S., R, B., Pal, A. K., Bagchi, S., Ghose, S. (2025). Peripheral ossifying fibroma: A case report. IP Int J Periodontol Implantol, 6(3), 179-183. https://doi.org/10.18231/j.ijpi.2021.031
MLA
Ghosh, Sandip, R, Balaji, Pal, Ashit Kumar, Bagchi, Somen, Ghose, Sandip. "Peripheral ossifying fibroma: A case report." IP Int J Periodontol Implantol, vol. 6, no. 3, 2025, pp. 179-183. https://doi.org/10.18231/j.ijpi.2021.031
Chicago
Ghosh, S., R, B., Pal, A. K., Bagchi, S., Ghose, S.. "Peripheral ossifying fibroma: A case report." IP Int J Periodontol Implantol 6, no. 3 (2025): 179-183. https://doi.org/10.18231/j.ijpi.2021.031
